My New Favorite Book to Increase Anxiety Tolerance: “Breath” by James Nestor
/I am so excited about a new book, Breath: The New Science of a Lost Art, by James Nestor.
Ok, I will admit that I am a little late to the party for the importance of breathing. Not that I was against breathing. I enjoy doing it every 5 to 10 seconds, but it has never been a therapy that I emphasize.
I’ve seen two challenges with breathing practices:
In the past, it has always been presented as either a mindfulness practice or an ecstatic practice. In these trainings, no one explained how to breathe in general.
When I explained to breathing practitioners that breathing practices increased anxiety in my patients with histories of trauma, no one had an explanation and they recommended that my patients ‘just hang in there'.
The challenge that people with complex trauma share is that focusing on slowing or controlling their breathing can create more anxiety, and then they feel like they are "failing" at breathing. Instead of a breathing practice,
Instead, I often have my patients name 3-5 colors that they can see around them. This allows the prefrontal cortex and the visual cortex to sit on the amygdala and slow the inner dialog, effectively lowering their anxiety. I thought that naming colors was the same neurological idea of breathing - just a different modality. Plus, I like being able to explain the neurophysiology: vision is at least 30% of our brain.
As a student of psychophysiology, I keep lists of physiology that cause mental health symptoms. When thinking about what can create the physical sensation of fear, independent from present or past emotional causes, I think about:
The amygdala being activated by the adrenaline released when the body needs to increase glucose, such as in hypoglycemia.
Nutrient deficiencies, such as protein, iron, and B vitamins.
The Vegas Nerve being mechanical pinched at the first and second cervical vertebrae (See Stanley Rosenburg's Book: Accessing the Healing Power of the Vagus Nerve: Self-Help Exercises for Anxiety, Depression, Trauma, and Autism.)
Now, I have a fourth item on my list: Carbon dioxide intolerance caused by survival breathing.
After reading Breath, I now think very differently about breathing as a tool for healing anxiety. James discusses how people can develop a narrow window of tolerance to carbon dioxide. He shares an example where a woman had no functional amygdala – so no fear responses to spiders, snakes, dangerous people... However, when she inhaled an air mixture with an increased carbon dioxide content, she had a full blow panic attack, and would NOT repeat the experiment.
What I had not appreciated, until reading this book, is that we have chemoreceptors in our brain and in our arteries that are monitoring for carbon dioxide and pH. As carbon dioxide builds up in our bloodstream, it triggers anxiety – sometimes high enough to create a full-blown panic attack.
But, if we don't have enough carbon dioxide in our systems, we can't properly oxygenate our bodies. With breathing patterns that keep carbon dioxide low, our tissues (muscles, digestive system, and brain) suffer from low oxygen states. We can develop fatigue, insomnia, sleep apnea, hypertension, cardiovascular disease, depression, anxiety, inflammation, auto-immune disease and have a weakened immune system. To be physically and mentally healthy, we need to have a range of carbon dioxide that we can tolerate. Studies indicate that people with anxiety have a very narrow range of carbon dioxide levels that they can handle (see links below).
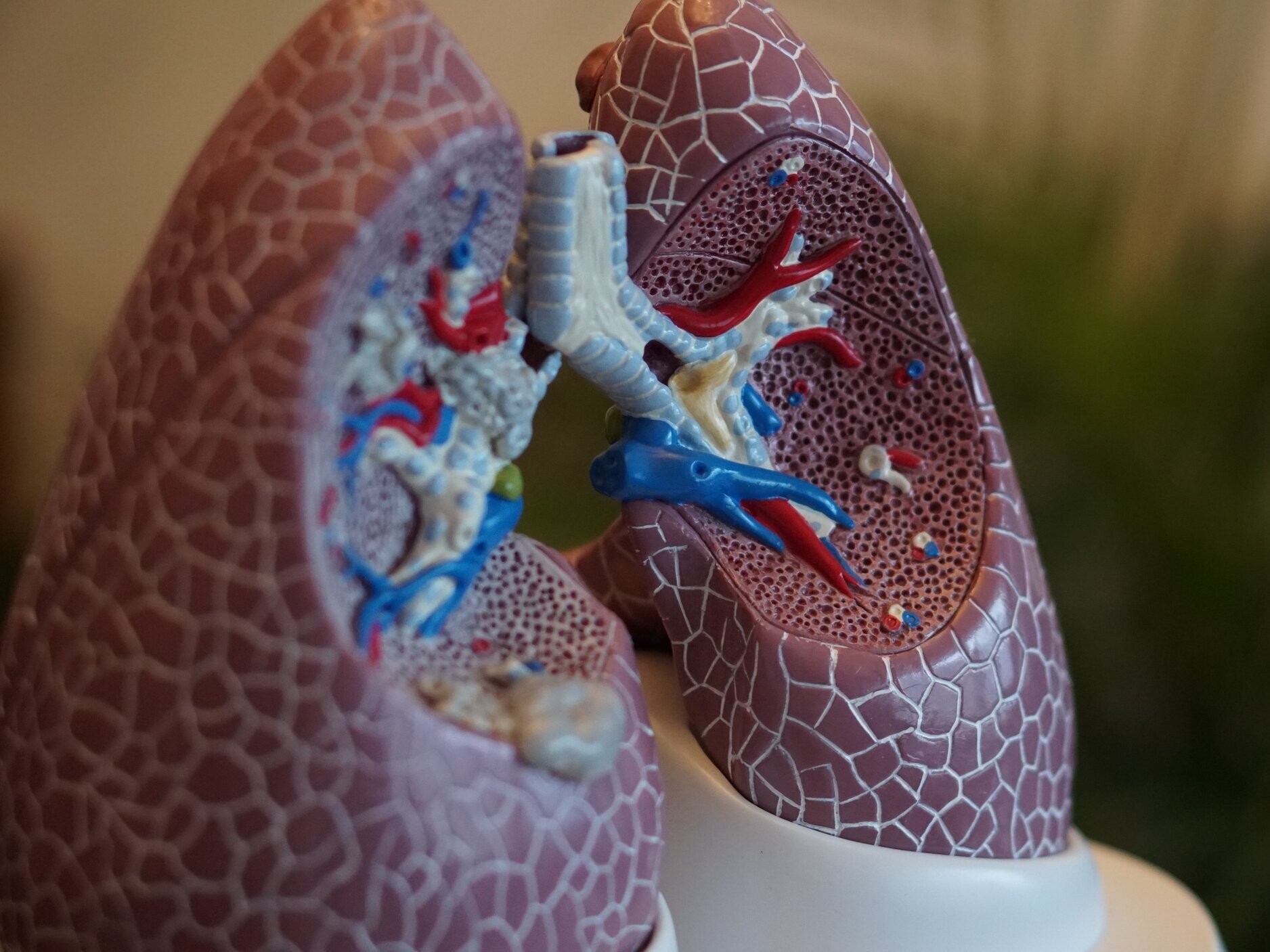
When we breathe through our mouths, we bring 20% less oxygen into our lungs. Breathing through our noses prepares the oxygen to be absorbed by the lungs into the red blood cells by removing bacteria, viruses, and particulates, increasing the humidity, and slowing the velocity of the molecules so that they can be absorbed into the capillaries carrying the red blood cells.
We need carbon dioxide present in the capillaries of the lungs so that it can exchange places with the oxygen in red blood cells. When we are intolerant of variations in carbon dioxide levels, we tend to breathe through our mouths. This lowers the carbon dioxide levels in our lungs and thereby lowers our oxygen absorption capacity. When we have lower oxygen levels in our bodies, we increase our bodies' stress, which increases our stress-related diseases.
However, what I was seeing when my patients focused on slowing their breathing was the impact of the increased levels carbon dioxide in their bloodstreams, causing an increased physical sense of anxiety (anxiety not caused by what is externally around them).
Now that I understand the physiological mechanism through which carbon dioxide can increase anxiety, I can more closely screen patients for behaviors that indicate that they may be avoiding the sensation anxiety created by carbon dioxide intolerance. These include:
Mouth breathing, while awake or while sleeping
Poor forward posture, often created by sitting in front of the computer
Hyperventilation (respiratory rates greater than 10 breaths per minute)
For the people with complex trauma, who often refuse to consider breathing techniques for their anxiety, I now start by explaining that they are not failing at breathing, but rather that they need to develop a slightly larger range of carbon dioxide tolerance. And that when they can tolerate more carbon dioxide, more oxygen will be available to their body, which will help them have more energy and mental clarity. Their brains will begin to wire in that higher levels of carbon dioxide is safe.
You might be wondering why we, as a species, are so hyper-vigilant to carbon dioxide when it’s so helpful in oxygenating our bodies. The carbon dioxide receptor is one of the oldest receptors found in most life forms. The earliest life forms on the planet were more concerned about getting into a space that was low in oxygen and high in carbon dioxide. This was a safety mechanism to stay alive, which was helpful in the past but not so helpful in our modern life.
Here are the steps that I am using to work with my patients around carbon dioxide intolerance;
Ask them to observe if they breathe through their mouths or noses. Times to observe are at work (particularly when working on a keyboard), watching screens, sleeping, and working out.
Ask them to focus on lightly closing their mouths when they can. This mindfulness practice will help them be aware of how they breath. When doing this, the patient might notice that they naturally breathe more deeply, using their whole rib cage. Suggesting that they place one hand on their chest and one hand on their belly is another way to help them see what muscles create their inhalation and exhalation. They might notice that they yawn more. I encourage focusing on their breath for at least 3 days, paying attention to what happens to their levels of energy and mental clarity. If they get anxious, they can breathe through their mouths for a time and then go back to breathing through their nose.
Even if they have a stuffy nose, still encourage them to try breathing through their noses. James Nestor, who suffered from allergies, a deviated septum, and often developed pneumonia, found that learning to breath through his nose actually improved these symptoms.
Ask if they are willing to lightly tape their mouths shut while sleeping, using a small piece of medical tape or KT tape – about the size of a postage stamp. It’s still easy to open their mouths if they need to, but it’s enough to remind them to keep their mouths shut and to breath through their noses. This decreases snoring and mild sleep apnea, and increases the oxygenation of their tissues.
Ask them to try keeping their mouths shut when working out. This will likely be uncomfortable at first, but if they persevere it can increase performance, endurance and recovery.
Lastly, ask them to think of breathing as a moment-to-moment practice that can take a lifetime to truly appreciate.
I hope this summary is helpful to you. Please feel free to email your questions. Your curiosity helps me learn to articulate the science in a usable fashion. Also feel free to share your own stories of breathing by commenting on this post below.
Related references:
Here a podcast interview with James Nestor, “How to Fix Your Breathing to Improve Your Health,” at Art of Manliness Podcast with Brett McKay #638 (46 minutes).
I listened to Breath on Audible. It was a fun book to listen with lots of stories and listening always make the science easier to hear for me.
Scientific Papers:
“Panic Attacks as a Problem of pH” by By Richard Maddock, May 18, 2010 in Scientific American
“The physiological effects of slow breathing in the healthy human”. by MA Russo, Santarelli DM, and O'Rourke D. in Breathe (Sheff). 2017;13(4):298-309.